Issues with lower wisdom teeth

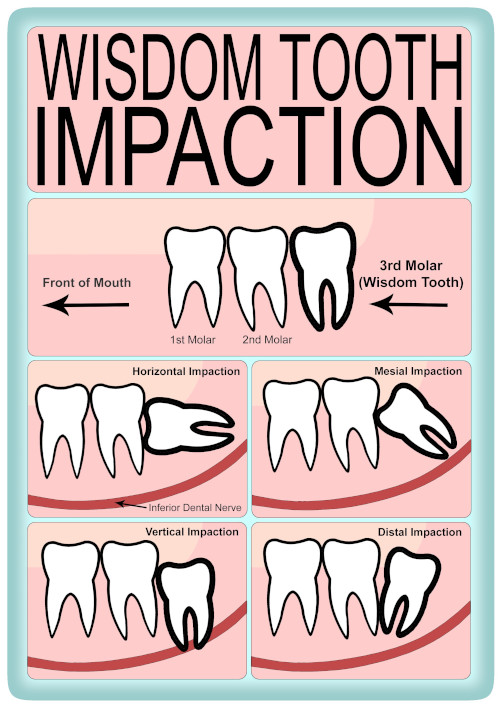
Wisdom teeth are the last teeth to develop in your jaws, often there is not enough space for them to erupt into the correct position like the other teeth in your mouth. They can vary in their position. Please see the image below for their different positions. Some may not erupt fully because they be impacted against another tooth or may be part covered by the gums (oral mucosa) A combination of this varied position, impaction, being partially erupted and other causes may create issues. You may not be aware that these are occurring.
One of the most common reasons you have been referred is that you’ve been having problems with your wisdom teeth. This may be due to pain, swelling or infection to the gum covering the wisdom tooth, also known pericoronitis. The wisdom tooth may also be decayed. You may also be getting food stuck around your wisdom teeth.
Some wisdom teeth may have no symptoms but there may be a problem developing or there is high risk of a problem developing that you may be unaware of. There is strong evidence to show that wisdom teeth that are mesially or horizontally positioned that have not erupted fully have a high risk of decay occurring within the wisdom tooth and also to the tooth in front. If left alone the decay may get to the extent that you may develop pain from both teeth. If the tooth in front is decayed it will need to be repaired by the Dentist after the wisdom tooth has been extracted.
The decay may get to the extent that the tooth in front has to be removed as well. The same may occur to the bone support around these teeth (periodontal disease). Sometimes cysts can form around the wisdom tooth. A cyst occurs when fluid fills the sack that normally surrounds a developing wisdom tooth and can slowly increase in size.

A horizontal wisdom impacted tooth.
There is early decay in the tooth in front.
Your dentist may be able to repair this tooth
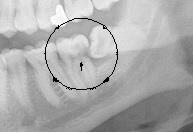
A horizontal impacted wisdom tooth.
There is extensive decay in the tooth in front.
Both teeth will need to be removed.
If you have a medical issue that requires you to start medicines such as immunosuppressants or medicines that affect the bone it is advisable to have an assessment of your teeth including your wisdom teeth before you start these medicines. If you were to have a tooth extracted while on these medicines this may slow down healing of a tooth socket. In rare cases the tooth socket may not heal at all. The assessment may recommend the need to remove teeth that are of a poor prognosis including your wisdom teeth.
If you are intending to travel abroad for a long length of time and access to a dentist or a specialist is difficult the consideration may be given about having treatment for your wisdom teeth and other teeth before you leave.
Do I need to be referred?
Some wisdom teeth can be straightforward to remove. Your Dentist might be able to remove them or may refer you to see a clinician who removes them routinely. You may need to go another Dental practice or a clinic in the community. They may be able to remove them on the same day as your first appointment.
For wisdom teeth that are difficult to remove or there are medical issues or if you wish to see a specialist, you may need to be referred to the hospital. The specialist will often be a Consultant in Oral and Maxillofacial Surgery or an Oral Surgeon. They will have the experience and qualifications to provide you with the information for you to decide about you would like to do about your wisdom teeth. Often the first appointment will be a consultation only and if necessary another appointment will be needed to have your treatment.
What options may be discussed?
There are several options about the management of your wisdom teeth.
No treatment but kept under review
If the wisdom tooth is in a position where it has not been causing problems and there is a low risk of a problem developing then an option can be for the wisdom tooth to be left where it is. Your Dentist can continue to review your wisdom teeth along with the rest of your teeth when you attend for your routine check up. When necessary your Dentist may need to take an X- ray of the wisdom teeth. However, over time circumstances may change and the risk of a problem with your wisdom teeth may increase, which treatment will then be needed. The time of when treatment is needed is a decision that can be made with you and the Dentist or the Specialist. It is important to keep your wisdom teeth under review as problems may develop with out you knowing about them until severe symptoms develop.
Treatment
In most cases where a problem has developed or a high risk of developing the wisdom tooth could be removed completely or part removed. During your consultation these options will be discussed with you in detail along with what is involved and the risks of the procedure. Your upper wisdom teeth may need to be removed as well.
What does the complete removal of lower wisdom teeth involve?
If the wisdom tooth has not fully erupted into the mouth it is often necessary to make a cut in the gum over the tooth. Sometimes it is also necessary to remove some bone surrounding the wisdom tooth. The tooth may need to be cut into 2 or 3 pieces to remove it. Once the wisdom tooth has been removed the gum is put back into place with stitches. In the majority of cases these stitches are dissolvable and take around two weeks to disappear.
What are the main possible risks of removing a wisdom tooth?
Most patients will recover fully with no problems.
- Bleeding
- There may be a little bleeding at the time of the extraction this usually stops very quickly and is unlikely to be a problem. If you are at home and the area bleeds again this can usually be stopped by applying pressure over the area for at least 10 minutes with a rolled up handkerchief or swab. If the bleeding does not stop, please contact the department where you had your operation.
- Altered Sensation to the chin, lower lip or tongue
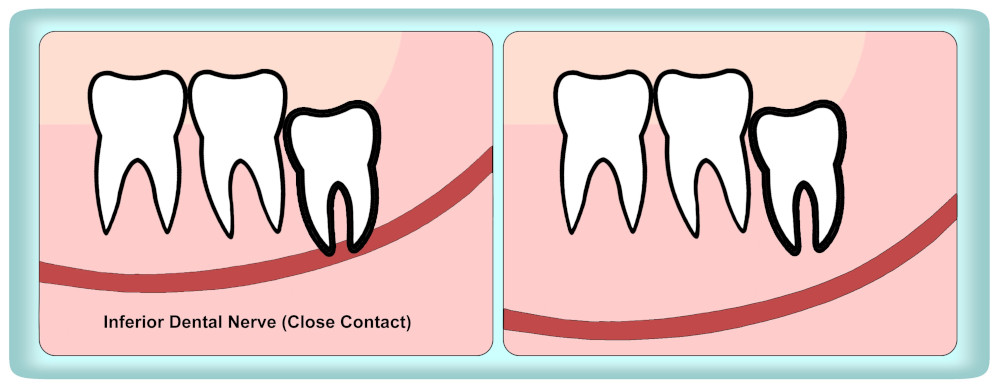
- Two nerves lie quite close to the lower wisdom teeth. The nerves can vary in their proximity to wisdom teeth. See the image below. The lingual nerve provides sensation in your tongue whilst the inferior dental nerve gives sensation to the lower lip and skin overlying the chin. Occasionally these nerves may be bruised during tooth removal. If this happens then you may have either numbness or pins and needles in either the tongue, lower lip, skin over the chin or any combination of these. If the wisdom tooth is away from the nerve the risk to the inferior dental nerve is less than 1%, however if the nerve is in very close contact the risk may be as high as 9%. The risk to the lingual nerve is less than 0.5%. It may take up to 18 months for this to recover. Rarely the nerve may not recover fully and you may be left with small patches of numbness to your lip or chin. Taste is rarely affected.
- Infection
- An infection in the in the socket can occur or the blood clot from extraction socket has dissolved away which may result in a dry socket. The incidence of this happening is low being in the order of 2%. It can be minimised by keeping the area clean with rinsing with water or a mouthwash starting this the day after your procedure. It is advisable not to smoke for a few days after having the wisdom tooth removed. Smoking can increase the risk of an infection or a dry socket. It may also be necessary for you to have a course of antibiotics after the extraction.
- Weakening of the Jaw
- In exceptional cases wisdom tooth removal can cause significant weakening of the jaw with the resultant possibility of jaw fracture. The incidence of this happening is extremely low and is less than 1% (less than 1 in 100).
A coronectomy
A coronectomy may be a treatment option. It may be offered if the inferior dental nerve in close contact to the wisdom tooth. In this technique only the upper portion of the wisdom tooth is removed leaving some of the tooth roots behind. This to minimise the risk of to the nerve. However, there is less than a 3% risk that you may need to have the remaining roots out at a later date or there may be delayed healing. At the consultation an assessment will be made to see to if this option is appropriate for you.
How long does it take to remove a wisdom tooth?
This is a variable. Some wisdom teeth may take only a few minutes to remove. More difficult wisdom teeth that need to be cut into pieces to remove can take around 20 minutes to extract.
Is there much pain or swelling after the removal of wisdom teeth?
It is likely that there will be some discomfort and swelling both on the inside and outside of your mouth after surgery. This is usually worse for the first three days but it may take up to two weeks before all the soreness goes. You may also find that your jaw is stiff and may not be able to open fully. You will need to eat a soft diet for a week or so. There may be some bruising of the skin of your face that can take up to a fortnight to fade away. The application of an ice pack during the first 24 hours post-operatively may help. Do not apply the ice pack directly to your skin - wrap the ice pack in a towel first. The older you are having a wisdom tooth removed the longer it will take to recover.
What type of anaesthetic is used?
A number of options are available and depend on how difficult the wisdom tooth is to remove
Local anaesthetic - this is an injection into gum surrounding the wisdom tooth, rather similar to that you may have had at your dentist for a filling. The injection takes a couple of minutes to numb the area and means that you will feel no pain while the wisdom tooth is removed.
Local anaesthetic and intravenous sedation – in addition to a local anaesthetic injection you can be given an injection into your arm. This makes you feel relaxed and less aware of the procedure. You are awake but patients frequently have little or no memory of the operation.
General anaesthetic – it is usually possible to remove wisdom teeth under a “day case” general anaesthetic, ie although you are put to sleep completely you will be able to go home on the same day as surgery.
Is there anything else I need to do after the extractions?
It is important to keep the extraction sites as clean as possible for the first few weeks after surgery. It may be difficult to clean your teeth around the sites of the extraction because it is sore and if this is the case it is best to keep the area free from food debris by gently rinsing with a mouthwash or warm salt water (dissolve a flat teaspoon of kitchen salt in a cup of warm water) commencing on the day after surgery.
Do I need to take any time off work?
Usually it will be necessary to take a few days off work and avoid strenuous exercise for this time. Depending on the type of anaesthetic used you may well not be able to drive (24 hours after intravenous sedation and for 48 hours after a general anaesthetic).
Further information
If you do want to know more about your operation please speak to your Dentist or the Specialist.
Here is a list of trusted websites that offer safe, sensible, useful information:
Royal College of Surgeons of England
British Association of Oral and Maxillofacial Surgeons
British Association of Oral Surgeons
NHS Stop Smoking Service.
NHS Choices
GOV.UK
DVLA - Driver and Vehicle Licensing Agency
Call 111 for non-emergency medical advice
